In my previous articles, I discussed 2 subjects that seems to be contradictory. On one hand, our microbiota, the good bacteria in the gut, help our body to fully use the food we eat. On the other hand, the immune system is programmed to destroy bacteria and other pathogens. The point is that for the benefits our microbiota brings to our body, the immune system is tolerant to the gut bacteria. Also, the bacteria are technically not inside the body but in the digestive tract, like a long tube passing through the whole body.
How the bacteria are kept away from the inside
Apart from the physical and immunological barriers mentioned in my previous article, mucus layers in the intestine are a good way to stop the bacteria from entering the body. Two different mucus layers are present in the intestinal lumen (aka the tube). The inner layer is quite tight (like jello). It starts at the head of the intestinal cells and is full of antimicrobial peptides (a kind of small protein) and antibodies. It prevents the microbiota to come too close from the intestinal cells and cross the barrier to enter the body. The outer layer is looser and is where all the good bacteria are present .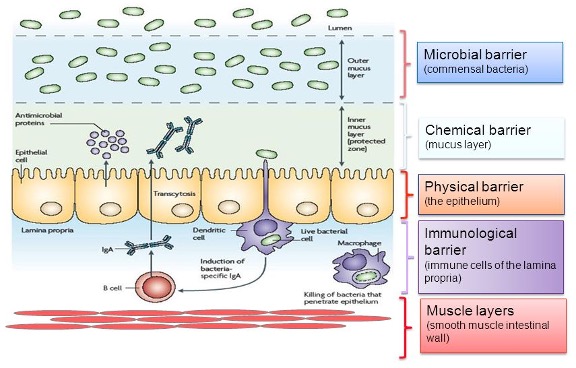
Benefits beats risks
While digesting complex fibers, the microbiota produces smaller molecules that can be absorbed by the intestinal cells. Those molecules are Bile Acids and Short-Chain Fatty Acids (SCFA). Primary Bile Acids are also naturally produced in the body and promote lipids (fat-rich food) absorption. Secondary Bile Acids are also essential to some natural body functions such as wound healing . SCFA can be used as body fuel but also improves antibody production and some immune functions. SCFA could also be protective against colon cancer.
Polysaccharides are present at the surface of certain bacteria. They are made of complex sugars and are recognized by our immune system. It is one of the ways, the immune system can stop the bacteria from invading the body. In the intestine, it is a little bit different because a lot of good bacteria are present. In that case, the recognition of specific polysaccharides by the immune cells produces T cells that are tolerant to the microbiota.
Balance is the key
As I mentioned in a previous article, T cells are divided in 2 main groups, but in reality, there are many small sub-groups (Th1, Th2, Th17, Tregs…). For the purpose of this article let’s class them as type I and type II. For the health of the immune system, perfect balance between type I and type II sub-groups is crucial. Type I is the default lineage of T helper cells when no antigen is present, or is created in the intestine as a T cell tolerant to the microbiota. Type II cells are created upon contact with a non-self molecule. If too many type II cells are present, an inflammatory disease may develop. In the opposite situation, you may develop autoimmune diseases as myasthenia gravis.
As crazy as it seems, the immune system and the microbiota need each other for our organism to function properly. A healthy microbiota will trigger the immune system just enough to keep it alert without pushing the balance towards over-reaction.
- Antoni, L et al. Intestinal barrier in inflammatory bowel disease, World Journal of Gastroenterology, 2014;20(5):1165-1179 [Accessed January 6, 2021]. Image mucus layers: https://www.weilab.com/weilab_condition_month.php?condition_id=102 [online December 29, 2020]
- Kayama H et al. Interaction Between the Microbiota, Epithelia, and Immune Cells in the Intestine. Annual Reviews of Immunology, 2020;38:23-48 [Accessed January 6, 2021]
- Round JL and Mazmanian SK. The gut microbiome shapes intestinal immune responses during health and disease, Nature Reviews Immunology, 2009;9(5):313-323 [Accessed January 6, 2021]